Professor H. Peter Soyer has been a trailblazer and leading figure in the field of dermatology for over 30 years. Since the mid 1980s, Prof. Soyer has focused on improving the early detection of melanoma, even playing a role in the first research project on dermoscopy.
In 2007, the Soyer family moved from Austria to Australia. Not only was this a welcome sea change, but it also presented Prof. Soyer with the opportunity to take his research to the next level; something he certainly did in his new role as Director of the Dermatology Research Centre at The University of Queensland Diamantina Institute.
A Mission to Make Melanoma Surveillance Photography More Accessible
Given Prof. Soyer’s passion for early melanoma detection, it should come as no surprise that the Diamantina Institute was the first site to join an innovative new clinical trial, coordinated by Melanoma and Skin Cancer Trials (MASC Trials).
The IMAGE trial is focused on Melanoma Surveillance Photography, a comprehensive surveillance method that combines 2D or 3D Total Body Photography (TBP) with digital dermoscopy to closely monitor skin lesions. The trial’s aim is to gather the evidence to determine whether TBP should be covered by Medicare to assist in the early detection of melanoma and reduce unnecessary ‘just in case’ biopsies.
“The idea behind melanoma screening is that you just don’t look at the individual lesion, but rather the whole body, because you don’t know where the melanoma is,” Prof. Soyer says.
While there are melanoma predilection sites — the back for men and legs for women — melanoma can occur anywhere on the body. Total body photography (or total body imaging) has the potential to be a game-changer in the early detection and treatment of skin cancer, as the full body images can be used for managing and tracking any potential changes over time.
The Power of Total Body Imaging
“It is so important to see the evolution of a person’s skin over time,” Prof. Soyer says.
“Imagine you have 20 moles; I see you now and I see you in a year, but without total body imaging, it’s difficult to know with certainty if a mole is new or not.”
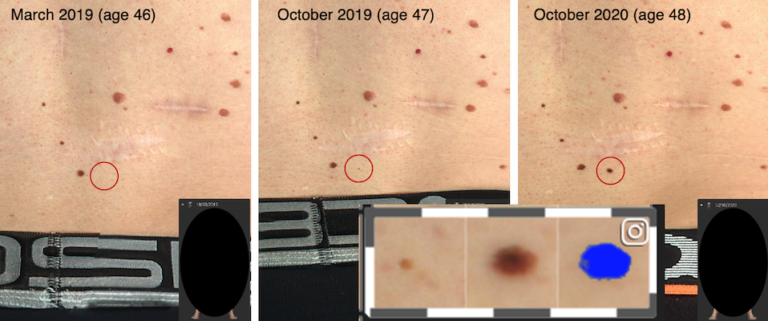
Prof. Soyer illustrates further with the case study of a man in his mid to late 40s with a history of melanoma. The patient was seen every month, over a period of 18 months, for total body imaging. As clearly shown below, a new mole appears on his back — a mole which easily could have been missed without a photographic baseline of the patient’s body.
A Vision for a Nationwide Melanoma Screening Program
Prof. Soyer is excited about the future of melanoma detection and treatment, with several trials and programs underway that could potentially see a paradigm shift in the field.
“I imagine a not-so-distant future where our smartphones are linked to AI-enhanced bathroom mirrors to alert us to any suspicious moles – but in the more immediate term, our vision is to establish a nationwide targeted melanoma screening program, particularly for people at high or ultra-high risk for melanoma,” he says.
Prof. Soyer knows that one of the biggest challenges in early detection is ensuring that regional and rural Australians will be able to access sites to undergo potentially life-saving melanoma surveillance photography.
MASC Trials’ IMAGE trial and other clinical trials, including The University of Queensland’s Australian Centre of Excellence in Melanoma Imaging & Diagnosis (ACEMID), hope to contribute towards making this vision a reality.
I imagine a not-so-distant future where our smartphones are linked to AI-enhanced bathroom mirrors to alert us to any suspicious moles – but in the more immediate term, our vision is to establish a nationwide targeted melanoma screening program, particularly for people at high or ultra-high risk for melanoma.
As Director of the MASC Trials Board, inaugural Chair and Director of The University of Queensland Dermatology Research Centre, and Director of the Princess Alexandra Hospital Dermatology Department, Prof. Soyer is a busy man. However, he shows no signs of slowing down!
If he’s not in the clinic or the lab (or rather the home office in these times), he’s likely to be hiking up his closest mountain or bushwalking with his wife.
Thank you to Prof. Soyer for not only generously sharing his time with us for this article, but also for his valuable contribution to MASC Trials and more broadly, the field of dermatology.
Glossary of Terms
- Melanoma – a type of cancer that develops in the skin’s pigment cells (melanocytes)
- Squamous cell carcinoma – a common type of skin cancer
- Basal cell carcinoma – a type of skin cancer that most commonly occurs on the face
- Dermatology – a branch of medicine concerned with the diagnosis and treatment of skin disorders
- Dermoscopy – a technique using a handheld device with a special lens (dermatoscope) that shows more features of a lesion than the human eye
- Lesion (as in skin lesion) – areas of skin that look different from the surrounding area
- Predilection site – common areas on the body where melanoma occurs
- Total Body Photography – images of the whole skin surface
About MASC Trials’ IMAGE Clinical Trial
Melanoma surveillance using Total Body Photography (TBP) is not currently subsidised by Medicare. The IMAGE clinical trial, led by A/Prof. Victoria Mar, aims to produce the evidence required by the Medical Services Advisory Committee to determine whether TBP should be reimbursed by Medicare.
The IMAGE trial is sponsored by Monash University and coordinated by the Melanoma and Skin Cancer Research Centre.

